| Pharmaceutical Information |
| Drug Name |
Dronedarone |
| Drug ID |
BADD_D00730 |
| Description |
Dronedarone is a Class III antiarrhythmic drug that works to restore the normal sinus rhythm in patients with paroxysmal or persistent atrial fibrillation. Atrial fibrillation is a common sustained arrhythmia where the treatment primarily focuses on stroke prevention and symptom management. It is managed by rate control, rhythm control, prevention of thromboembolic events, and treatment of the underlying disease.[A34604] Similar to [amiodarone], dronedarone is a multichannel blocker that works to control rhythm and rate in atrial fibrillation.[A186071] It meets criteria of all four Vaughan Williams antiarrhythmic drug classes by blocking sodium, potassium, and calcium ion channels and inhibiting β-adrenergic receptors.[A34604,L8699]
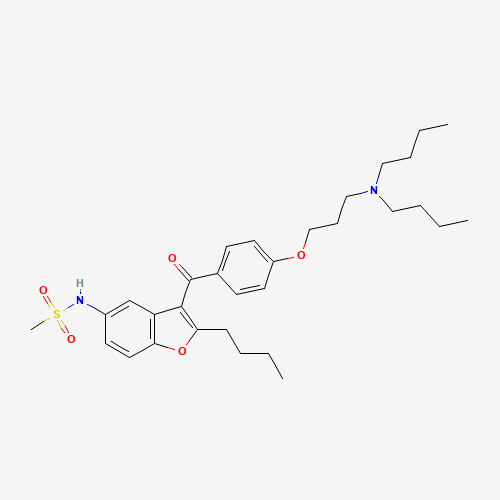
Dronedarone is a related benzofuran compound to amiodarone but its chemical structure lacks iodine moieties which are associated with amiodarone-induced thyroid problems.[A34604,T28] Additionally, the methyl sulfonyl group in its structure renders dronedarone to be more lipophilic with a shorter half-life than amiodarone.[A34604] This ultimately leads to reduced tissue accumulation of the drug and decreased risk for organ toxicities, such as thyroid and pulmonary toxicities.[T28] Commonly marketed as Multaq®, dronedarone was approved by the FDA in July 2009 and Health Canada in August 2009. A safety concern for the risk of drug-induced hepatocellular injury has been issued following marketing of dronedarone.[L8800] |
| Indications and Usage |
Dronedarone is indicated for the management of atrial fibrillation (AF) in patients in sinus rhythm with a history of paroxysmal or persistent AF to reduce the risk of hospitalization.[L8699] |
| Marketing Status |
approved |
| ATC Code |
C01BD07 |
| DrugBank ID |
DB04855
|
| KEGG ID |
D02537
|
| MeSH ID |
D000077764
|
| PubChem ID |
208898
|
| TTD Drug ID |
D05CPV
|
| NDC Product Code |
53360-4142; 0024-4142; 55154-8104 |
| UNII |
JQZ1L091Y2
|
| Synonyms |
Dronedarone | Multaq | SR 33589B | SR 33589 |
|
| Chemical Information |
| Molecular Formula |
C31H44N2O5S |
| CAS Registry Number |
141626-36-0 |
| SMILES |
CCCCC1=C(C2=C(O1)C=CC(=C2)NS(=O)(=O)C)C(=O)C3=CC=C(C=C3)OCCCN(CCCC)CCCC |
| Chemical Structure |
|
|
| ADRs Induced by Drug |
|
|
*The priority for ADR severity classification is based on FAERS assessment, followed by the most severe level in CTCAE rating. If neither is available, it will be displayed as 'Not available'.
**The 'Not Available' level is hidden by default and can be restored by clicking on the legend twice..
|
|
|

