| Pharmaceutical Information |
| Drug Name |
Insulin detemir |
| Drug ID |
BADD_D01162 |
| Description |
Insulin detemir is a long-acting form of insulin used for the treatment of hyperglycemia caused by Type 1 and Type 2 Diabetes. Insulin is typically prescribed for the management of diabetes mellitus to mimic the activity of endogenously produced human insulin, a peptide hormone produced by beta cells of the pancreas that promotes glucose metabolism. Insulin is released from the pancreas following a meal to promote the uptake of glucose from the blood into internal organs and tissues such as the liver, fat cells, and skeletal muscle. Absorption of glucose into cells allows for its transformation into glycogen or fat for storage. Insulin also inhibits hepatic glucose production, enhances protein synthesis, and inhibits lipolysis and proteolysis among many other functions.
Insulin is an important treatment in the management of Type 1 Diabetes (T1D) which is caused by an autoimmune reaction that destroys the beta cells of the pancreas, resulting in the body not being able to produce or synthesize the insulin needed to manage circulating blood sugar levels. As a result, people with T1D rely primarily on exogenous forms of insulin, such as insulin detemir, to lower glucose levels in the blood. Insulin is also used in the treatment of Type 2 Diabetes (T2D), another form of diabetes mellitus that is a slowly progressing metabolic disorder caused by a combination of genetic and lifestyle factors that promote chronically elevated blood sugar levels. Without treatment or improvement in non-pharmacological measures such as diet and exercise to lower blood glucose, high blood sugar eventually causes cellular resistance to endogenous insulin, and in the long term, damage to pancreatic islet cells. Insulin is typically prescribed later in the course of T2D, after several oral medications such as [DB00331], [DB01120], or [DB01261] have been tried, when sufficient damage has been caused to pancreatic cells that the body is no longer able to produce insulin on its own.
Marketed as the brand name product Levemir, insulin detemir has a duration of action of 16-24 hours allowing for once-daily dosing, typically at bedtime. Due to its duration of action, Levemir is considered "basal insulin" as it provides low concentrations of background insulin that can keep blood sugar stable between meals or overnight. Basal insulin is often combined with short-acting "bolus insulin" such as [DB00046], [DB01309], and [DB01306] to provide higher doses of insulin required following meals. Use of basal and bolus insulin together is intended to mimic the pancreas' production of endogenous insulin, with a goal of avoiding any periods of hypoglycemia.
Insulin detemir is produced using recombinant DNA technology in yeast cells. This insulin analogue has a 14-C fatty acid, myristic acid, bound to the lysine amino acid at position B29. The myristoyl side chain increases self-association and albumin binding. This along with slow systemic absorption from the injection site prolongs distribution of the hormone into tissues and results in a long duration of action.
Without an adequate supply of insulin to promote absorption of glucose from the bloodstream, blood sugar levels can climb to dangerously high levels and can result in symptoms such as fatigue, headache, blurred vision, and increased thirst. If left untreated, the body starts to break down fat, instead of glucose, for energy which results in a build-up of ketone acids in the blood and a syndrome called ketoacidosis, which is a life-threatening medical emergency. In the long term, elevated blood sugar levels increase the risk of heart attack, stroke, and diabetic neuropathy. |
| Indications and Usage |
Insulin detemir is indicated to improve glycemic control in adults and children with diabetes mellitus. |
| Marketing Status |
approved |
| ATC Code |
A10AE05 |
| DrugBank ID |
DB01307
|
| KEGG ID |
D04539
|
| MeSH ID |
D000069057
|
| PubChem ID |
16137271
|
| TTD Drug ID |
D0QE5U
|
| NDC Product Code |
0169-6432; 50090-6391; 0420-9013; 0169-3687; 0420-9003; 50090-1276; 0169-6438; 50090-6414; 50090-1475 |
| UNII |
4FT78T86XV
|
| Synonyms |
Insulin Detemir | Detemir, Insulin | Basal Insulin Detemir | Detemir, Basal Insulin | Insulin Detemir, Basal | NN304 | NN-304 | NN 304 | B29-tetradecanoyl-Lys-B30-des-Ala-insulin | B29 tetradecanoyl Lys B30 des Ala insulin | Insulin, Tetradecanoyl-Lys(B29)-des-Ala(B30) | 12C-Lys(B29)-DB30I | Des-(B30)-insulin, Lys(B29)-tetradecanoyl | Insulin, Tetradecanoyllysyl(B29)-desalanyl(B30) | Levemir |
|
| Chemical Information |
| Molecular Formula |
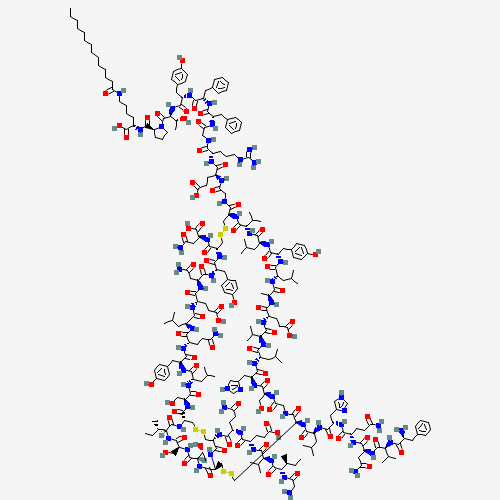
C267H402N64O76S6 |
| CAS Registry Number |
169148-63-4 |
| SMILES |
CCCCCCCCCCCCCC(=O)NCCCCC(C(=O)O)NC(=O)C1CCCN1C(=O)C(C(C)O)NC(=O)C(CC2=CC=C(C=C2)
O)NC(=O)C(CC3=CC=CC=C3)NC(=O)C(CC4=CC=CC=C4)NC(=O)CNC(=O)C(CCCNC(=N)N)NC(=O)C(CC
C(=O)O)NC(=O)CNC(=O)C5CSSCC(NC(=O)C(NC(=O)C(NC(=O)C(NC(=O)C(NC(=O)C(NC(=O)C(NC(=
O)C(NC(=O)C(NC(=O)C6CSSCC(C(=O)NC(CSSCC(C(=O)NCC(=O)NC(C(=O)NC(C(=O)NC(C(=O)NC(C
(=O)NC(C(=O)NC(C(=O)NC(C(=O)NC(C(=O)NC(C(=O)NC(C(=O)N5)C(C)C)CC(C)C)CC7=CC=C(C=C
7)O)CC(C)C)C)CCC(=O)O)C(C)C)CC(C)C)CC8=CNC=N8)CO)NC(=O)C(CC(C)C)NC(=O)C(CC9=CNC=
N9)NC(=O)C(CCC(=O)N)NC(=O)C(CC(=O)N)NC(=O)C(C(C)C)NC(=O)C(CC1=CC=CC=C1)N)C(=O)NC
(C(=O)NC(C(=O)NC(C(=O)N6)C(C)CC)CO)C(C)O)NC(=O)C(CCC(=O)N)NC(=O)C(CCC(=O)O)NC(=O
)C(C(C)C)NC(=O)C(C(C)CC)NC(=O)CN)CO)CC(C)C)CC1=CC=C(C=C1)O)CCC(=O)N)CC(C)C)CCC(=
O)O)CC(=O)N)CC1=CC=C(C=C1)O)C(=O)NC(CC(=O)N)C(=O)O |
| Chemical Structure |
|
|
| ADRs Induced by Drug |
|
|
*The priority for ADR severity classification is based on FAERS assessment, followed by the most severe level in CTCAE rating. If neither is available, it will be displayed as 'Not available'.
**The 'Not Available' level is hidden by default and can be restored by clicking on the legend twice..
|
|
|

